Most of our intended parents (i.e., recipients) are age 35 or older, and about half of TSBC births are to recipients in this age range. While it is true that being over 35 brings a particular set of challenges when trying to conceive, we know that these challenges can often be overcome with advance planning and information.
As you age, the chance of conceiving decreases and the less time you have to try. For this reason, if you are in your mid-30s or older, we recommend that you have your fertility evaluated by a medical professional specializing in reproduction. A fertility evaluation will give you valuable information that may impact the decisions you make when trying to conceive.
TSBC data
This figure shows the conception rate in a cycle attempt. Recipients are grouped by age and whether they inseminated vaginally (VP) or used intrauterine insemination (IUI).
Based on 5 years of data (2012-2017), for all recipients combined, the overall conception rate per cycle attempt for IUI was 20.9% (birth rate 15.1%) and for vaginal insemination was 7.9% (birth rate 5.3%).
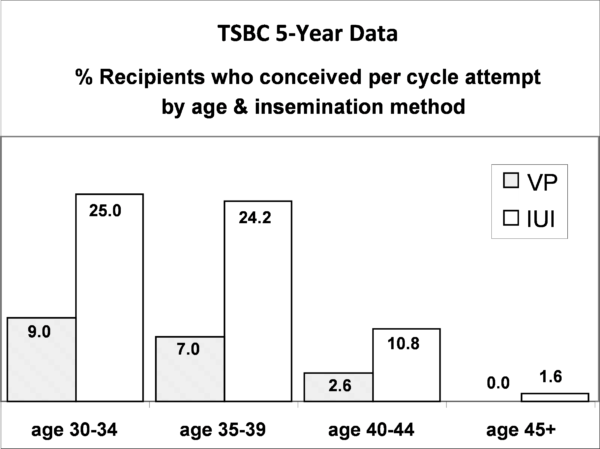
Conception rates were closely related to recipient age. Looking at recipients aged 40-42, results from IUIs were reasonable, with a 1 in 10 chance of conceiving in a cycle attempt. If you do not conceive via IUI within 2-3 cycle attempts, especially if you are 40+, we recommend that you consult a fertility specialist.
Many of our recipients are reluctant to use fertility drugs or other interventions until they have tried a few natural cycles. This is understandable, and we encourage you to create an insemination plan that feels comfortable to you, prior to when you begin trying to conceive.
Make a timeline
Below are suggestions on how to create both a realistic and comfortable insemination plan.
- We recommend everyone have a preconception counseling session with a medical professional before trying to conceive. Your provider may recommend testing before you start trying. Assessing your fertility early, and again at the specific times frames below, may increase your chance of success and decrease the time (and financial cost) it takes you to conceive.
- If you are between the ages of 35 and 39, we encourage you to consult with a reproductive specialist after you have inseminated for three to six cycles without conceiving.
- If you are between the ages of 40 and 42, we advise you to consult with a reproductive specialist after two or three unsuccessful cycle attempts.
- If you are between the ages of 43 and 44, we highly recommend that you seek reproductive specialist advice before you begin the insemination process.
- Statistics suggest that by age 43, people have less than a 10% chance of conceiving with their own eggs, 90% of which are chromosomally abnormal at this point. While it is not impossible to conceive and carry to term at this age, early medical evaluation can help you avoid wasting valuable fertile time.
- If you are 44 or older, we strongly suggest that you consider using a donor egg or embryo, as the odds of successful conception with your own eggs are now very low. Of the more than 4000 births reported to TSBC from 1982-2017, 8 (0.2%) have been to recipients 45+ who conceived with their own eggs. Of these 8, 7 conceived in the first three cycle attempts. Age-related decline in fertility is almost exclusively caused by aging in the egg follicles, not by aging of the uterus, so for many recipients it is possible to become pregnant and deliver a healthy baby with the help of an egg donor.
Other considerations
- Consider additional testing. The Day 3 test is the most common test used to evaluate fertility. This simple blood test looks at the levels of Follicle Stimulating Hormone (FSH) and Estradiol (estrogen produced by the ovaries) in your bloodstream on the third day of your cycle. If these levels are too high, it indicates that your endocrine system is working too hard to stimulate the development of egg follicles, and suggests a diminished ovarian reserve. High levels don’t necessarily indicate that you can’t conceive; but they do indicate that you may want to consider using fertility drugs to increase your chance of conceiving.
- Another helpful test assesses progesterone level about one week after ovulation. It will indicate if you’ve ovulated.
- Consider medicated cycles with fertility drugs like Clomid, Progesterone, or Gonadotropins. Consult with a fertility specialist.
- Consider In Vitro Fertilization (IVF) with your fertility specialist. It may increase the chance of conceiving.
Alternative treatments for fertility
Some recipients prefer to try alternative treatments for fertility before, in addition to, or instead of western medical treatments. Alternative treatments to increase fertility can include acupuncture and traditional Chinese medicine, Chinese herbs or other herbal supplements, Mind-Body programs, and special diet or exercise programs. There are fewer scientific studies on the outcome of these treatments and the existing studies conflict about whether they benefit. However, evidence of success is building for Mind-Body programs, consistent with some TSBC recipient reports.
Emotional and psychological support
Trying to conceive can be stressful, especially for recipients with age-related concerns. Each month can be an emotional roller coaster. This can be further compounded for recipients who choose to keep their decision to inseminate private or who are taking fertility medications such as those discussed above. Many find it helpful to seek out the emotional support of a few close friends, a support group, and/or a trained counselor. When facing challenging conceptions, having caring, understanding people to talk to about your feelings and experiences becomes even more important. We encourage you to evaluate your support system and take steps to ensure that you have adequate emotional and psychological support throughout the insemination process.
